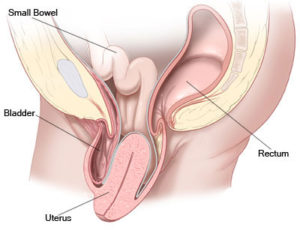
When the muscles and ligaments supporting a woman’s pelvic organs weaken, the pelvic organs uterus can slip out of place (prolapse). Pelvic organ prolapse can worsen over time, and you may need surgery to fix it. There are different types of pelvic organ prolapse. Some women develop pelvic organ prolapse after childbirth, or hysterectomy vault prolapse.
Anterior prolapse, also known as a cystocele (SIS-toe-seel), occurs when the supportive tissue between a woman’s bladder and vaginal wall weakens and stretches, allowing the bladder to bulge into the vagina. Anterior prolapse is also called a prolapsed bladder.
Straining the muscles that support your pelvic organs may lead to anterior prolapse. Such straining occurs during vaginal childbirth or with chronic constipation, violent coughing or heavy lifting. Anterior prolapse also tends to cause problems after menopause, when estrogen levels decrease.
For a mild or moderate anterior prolapse, nonsurgical treatment is often effective. In more severe cases, surgery may be necessary to keep the vagina and other pelvic organs in their proper positions.
In mild cases of anterior prolapse, you may not notice any signs or symptoms. When signs and symptoms occur, they may include:
Signs and symptoms often are especially noticeable after standing for long periods of time and may go away when you lie down.
If self-care measures aren’t effective, anterior prolapse treatment might involve:

A posterior prolapse occurs when the thin wall of fibrous tissue (fascia) that separates the rectum from the vagina weakens, allowing the vaginal wall to bulge. Posterior prolapse is also called a rectocele (REK-toe-seel) because typically, though not always, it’s the front wall of the rectum that bulges into the vagina.
Childbirth and other processes that put pressure on the fascia can lead to posterior prolapse. A small prolapse may cause no signs or symptoms. If a posterior prolapse is large, it may create a noticeable bulge of tissue through the vaginal opening. Though this bulge may be uncomfortable, it’s rarely painful
A small posterior prolapse may cause no signs or symptoms. Otherwise, you may notice:
If the posterior prolapse protrudes outside your vagina and is especially bothersome, you may opt for surgery. Surgery to repair posterior prolapse will repair the tissue bulge, but it won’t fix impaired bowel function. Your doctor will likely suggest surgery if you have prolapse of other pelvic organs in addition to posterior prolapse. Surgical repair for each condition can be completed at the same time.
Using a vaginal approach, surgery usually consists of removing excess, stretched tissue that forms the posterior prolapse. Occasionally, the surgical repair may involve using a mesh patch to support and strengthen the wall between the rectum and vagina.


Uterine prolapse occurs when pelvic floor muscles and ligaments stretch and weaken, providing inadequate support for the uterus. The uterus then slips down into or protrudes out of the vagina.
Uterine prolapse can happen to women of any age, but it often affects postmenopausal women who’ve had one or more vaginal deliveries. Weakening of the pelvic muscles that leads to uterine prolapse can be caused by:
Uterine prolapse varies in severity. You may have mild uterine prolapse and experience no signs or symptoms. If you have moderate to severe uterine prolapse, you may experience:
Weakening of pelvic muscles and supportive tissues contribute to uterine prolapse. This may happen as a result of:
To repair damaged or weakened pelvic floor tissues, your surgeon may perform the procedure through your vagina, although sometimes an abdominal surgery is needed. Surgical repair of your prolapse may involve grafting your own tissue, donor tissue or some synthetic material onto weakened pelvic floor structures to support your pelvic organs. Your surgeon may recommend a hysterectomy, which removes your uterus.
In some cases, minimally invasive (laparoscopic) surgery is a possibility.
This procedure involves smaller abdominal incisions, special surgical instruments and a lighted camera-type device (laparoscope) to guide the surgeon.